Obesity is an epidemic in the United States. As a disease, obesity has become associated with several co-morbidities or health conditions that decrease the quality of life and increase the risk of dying. Researchers know a connection exists between obesity and cancer, as being overweight or obese increases your risk for several types of cancer. However, what is not clear is how being obese increases that risk.
Maintaining a healthy weight is essential to overall health, so many people try one diet after another to lose weight. Unfortunately, many people end up yo-yo dieting, achieving some weight loss, only to regain even more. Some overweight people turn to bariatric surgery to reduce cancer and other comorbid health conditions when diets don’t work.
What is Obesity?
Obesity is a disease where a person has an unhealthy amount of body fat tissue. Those who are overweight or obese often have metabolic syndrome problems at a younger age, including coronary heart disease, type 2 diabetes, high blood pressure, and sleep apnea, to name a few chronic conditions.
A measurement called body mass index (BMI) determines your level of obesity. Body mass index is based on your weight and height. Your classification can vary, depending on your race and body makeup, as more muscular individuals weigh more than those with excess fat cells. Scientists use BMI to help understand how excess weight relates to cancer, but it does not predict future health.
A healthy body mass index is generally between 18.5 and 24.9, while a BMI between 25 and 29.5 is considered overweight. If your body mass index is 30 or higher, you are considered obese.
Those who have a BMI of 40.0 or high are considered severely obese. To determine your BMI, divide your weight in pounds by your height in inches. For example, an individual who is 5 foot, 6 inches, or 66 inches tall and weighs 180 lbs. would have a BMI of 29.0. You can easily calculate your body mass index here.
Sometimes, doctors use measurements that reflect body fat distribution along with BMI to indicate obesity and disease risks. These include waist circumference, waist-to-hip ratio, waist-to-height ratio, and fat distribution measured by dual-energy X-ray absorptiometry to CT or PET scans.
Research indicates that larger waist measurements have a higher risk of cancer. A healthy waist measurement is under 40 inches for men and under 35 inches for women.
How Does Obesity Increase Cancer Risk?
The evidence linking obesity with cancer comes primarily from studied patient cohorts. Medical experts believe that visceral fat cells that largely surround your vital organs cause inflammation, leading to increased cancer risk.
The main problem with excessive visceral fat is that it affects specific processes, including how the body manages hormones such as insulin and estrogen.
Visceral fat cells are large. This excess fat has little room for oxygen, which triggers inflammation, the body’s natural response to injury and disease. Inflammation can increase cancer risk by affecting how and when cells divide and die. Cancer cells reproduce uncontrollably and damage nearby cells, causing illness. As more cells divide and multiply, the risks increase, leading to the development of tumor cells.
Inflammation and Insulin
The evidence to link obesity, inflammation, and insulin, the hormone that regulars blood sugar, is complex. Inflammation caused by obesity can keep your body from appropriately responding to insulin.
When the body doesn’t respond correctly, it produces more insulin. This increase due to insulin resistance triggers an increase n the number of cells produced and can also affect how hormones like estrogen are controlled.
Obese individuals often have increased blood levels of insulin and insulin-like growth factor (IGF-1), which usually precedes the development of type 2 diabetes, another known cancer risk factor. High levels of insulin and insulin-like growth factor may lead to kidney, colon, endometrial, and prostate cancer development.
Chronic inflammatory conditions like gallstones or non-alcoholic fatty liver disease can cause oxidative stress, leading to DNA damage and an increased risk for the biliary tract and other cancers.
Excess Estrogen
Fat cells may also, directly and indirectly, affect other cell growth and metabolic regulators, including producing excess estrogen. Higher estrogen levels lead to increased cell production, which could result in tumor growth.
Fat cells can also make estrogen in addition to the ovaries in women and an enzyme in men that converts testosterone in men. Excess estrogen is linked to postmenopausal breast cancer and endometrial and ovarian cancers in women.
In addition to biological mechanisms linking obesity with cancer, being overweight can lead to difficulties in screening and cancer management.
Overweight and obese women have an increased risk of cervical cancer than those with a healthy weight because of less effective cancer screening in these individuals.
What Research is Being Done on Obesity and Cancer?
Current studies are exploring many different mechanisms that link obesity and cancer. One area involves the role of microbes that live in the gastrointestinal tract of those with both type 2 diabetes and obesity.
Both health issues are associated with dysbiosis, an imbalance of these microbes. These imbalances may cause inflammation, altered metabolism, and genotoxicity, which may result in cancer.
Cancer research has also delved into how obesity alters the tumor microenvironment, possibly affecting cancer progression. Another area involves the role of insulin receptors in signaling cancer. Many cancer cells have elevated levels of IR-A, a form of this receptor with a high affinity for insulin and related growth factors.
Research focuses on how these factors contribute to metabolic syndrome and cancer risk and whether they may be used for therapeutic interventions to prevent obesity-related cancers.
The National Cancer Institute Consortium gathers prospectively studied cohort information from around the world, focusing on details like body mass index, waist circumference, and similar measures.
The large consortium size will allow researchers to understand better how obesity relates to less common cancers like those affecting the thyroid, gallbladder, kidney, and head and neck.
Another area focuses on developing more precise and effective ways to prevent weight regain after weight loss.
These include National Institutes of Health initiatives which aim to identify predictors of successful weight loss and maintenance and to incorporate information on genetic, psychosocial, behavioral, biological, and environmental factors. NCI supports research on obesity and cancer risk through various means.
How Common is Obesity and Severe Obesity?
Obesity has become increasingly common in the United States over the last decade, with the recent Covid-19 pandemic apparently worsening the problem. In 2011, 27.4% of adults ages 18 and older had obesity or severe obesity; in 2020, that percentage had increased to 31.9%.
The Centers for Disease Control (CDC) indicates that obesity differs among racial and ethnic groups. The figures for 2020 were as follows:
- Non-Hispanic Black, 41.6%
- Native American, 38.8%
- Hawaiian/Pacific Islander, 38.5%
- Hispanic, 36.6%
- Non-Hispanic White, 30.7%
- Asian, 11.7%
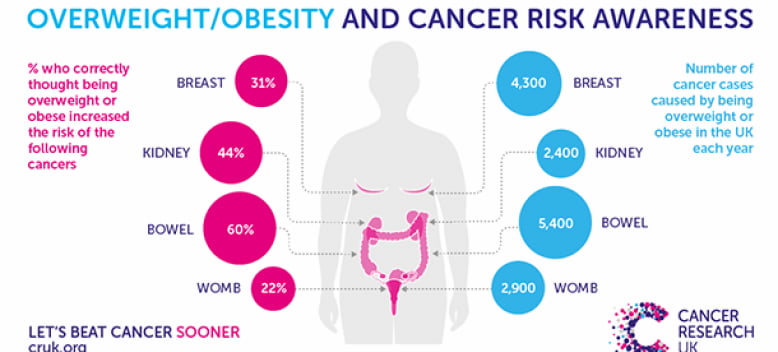
What Types of Cancer Have Links to Obesity or Being Overweight?
The following types of cancer types have links to being overweight or obese:
- Breast
- Uterine
- Ovarian
- Prostate
- Pancreas
- Gallbladder
- Liver
- Thyroid
- Colorectal
- Head and neck
- Esophagus
- Meningioma
- Multiple myeloma
Being overweight or obese has particular consequences for post-menopausal breast cancer and increases the cancer risk for other female cancers, as weight gain often increases after menopause.
However, other factors can also contribute. Hormone changes, gene mutations, long-lasting infections, and tobacco and alcohol use can also affect cancer risk.
Being overweight or having obesity doesn’t mean you will definitely develop cancer, but it indicates you are more likely to receive a cancer diagnosis at some point than someone who maintains a healthy weight.
How Many Cancer Cases Result from Obesity?
The United States Cancer Statistics database has estimated from a cross-sectional study using body mass index and cancer incidence data that about 37,360 new cancer cases in men and 74,690 new cancer cases in women resulted annually from 2011 to 2015 due to excess body weight.
The incidence was as high as 51% for liver and gallbladder cancers, while the rate was 49.2% for endometrial cancer in women. A 2019 global study found that excess body weight accounted for approximately 3.9% of all cancers in 2012, with more obesity-related cancers occurring in women than men because of obesity.
From 2005 to 2014, most cancers associated with overweight and obesity increased in the United States, while cancers associated with other factors decreased.
During this time, new cancers increased by 7%, while new cancers not associated with overweight and obesity dropped by 13%. The rate of new colorectal cancer cases dropped by 23% during this time.
How Does Obesity Affect Cancer Survivors?
Most evidence about obesity in cancer survivors comes from those diagnosed with breast, prostate, or colorectal cancer. Cancer research indicates that obesity may worsen several aspects of survivorship, including cancer recurrence, progression, prognosis, and the risk of some second primary cancers.
Such problems can include increased risk factors for lymphedema in breast cancer survivors and incontinence in prostate cancer survivors.
In a large clinical trial of patients with stage II and stage III colorectal cancer, those with a higher baseline body mass index, especially men, had an increased risk of local recurrence. Death from multiple myeloma is 50% higher for those with the highest levels of obesity.
Maintain Weight for Cancer Prevention
Cancer research shows that even if you and your doctors believe you have a healthy body weight, you can take steps to maintain it and decrease your cancer risk:
- Avoid a high-fat diet
- Primarily eat vegetables, fruits, lean proteins, and whole grain
- Consume foods that make you feel full, including healthy fats like nuts, fish, and olive oil
- Avoid highly processed foods like lunch meats, chips, white bread, cookies, and packaged foods with artificial ingredients
- Limit sugary drinks like fruit juice and soda
Increase Physical Activity
Whether you have a healthy weight or are overweight or obese, increased physical activity can help decrease your cancer risk. The Centers for Disease Control (CDC) recommend that adults get 150 minutes of moderate-to-intense aerobic activity per week, plus two days of strength training. Increasing your physical activity with something you love, like walking, swimming, etc., is part of a weight loss program that can also help avoid problems like cardiovascular disease and having too much extra weight.
Reducing an Elevated Cancer Risk If you are Overweight or Obese
Eating well and being more active are the best ways to improve your health if you are overweight or obese. Losing as little as 5% to 10% of your total body weight can reduce your risk of developing cancer.
Obesity and cancer research show that it can improve your health, too. Even if you find losing weight difficult, eating a more balanced diet and exercising regularly helps lower your cancer risk.
Try doing the following to reduce your risk factors.
Start With Small Changes
If you struggle with diet and exercise, ask your doctor for recommendations. Make initial changes small and achievable. Work with individuals like a nutritionist, exercise specialist, psychologist, doctor specializing in weight loss, and similar professionals who can help you make changes.
Find a Weight Loss Program With Support
When losing weight, getting the proper support is essential. The best weight loss programs include sessions with a dietitian or weight loss specialist.
They can help you make healthier changes and stick with them over time to avoid weight gain. Talk to your family about the changes you want to make and ask them for help.
Consider Medication for Losing Weight
Ask your healthcare provider if weight loss medication is an option for you. An increasing number of weight loss medications are now available for patients with difficulty losing weight through diet and exercise.
Is Weight Loss after a Cancer Diagnosis Beneficial for Those Who are Overweight or Obese?
Most studies on this question have focused on breast cancer. Several clinical trials in breast cancer survivors have reported that weight loss resulted in beneficial changes in biomarkers linked to cancer prognosis. However, little evidence exists about whether weight loss reduces breast cancer risk for recurrence or death.
Is Bariatric Surgery for You?
Because obesity is a disease, no matter what some patients do, they can’t lose weight and fat tissue and may even experience additional weight gain. If you cannot achieve weight loss and have started to develop cardiovascular disease, and type 2 diabetes, you may want to consider weight loss surgery. Bariatric surgery is an option for people who have a body mass index of 35 or more with one or more severe health conditions. Some doctors even recommend bariatric surgery if your body mass index is lower and you have a family history of obesity and cancer risk factors.
Work with your healthcare team to make healthy changes and lose weight. A cycle of yo-yo dieting, where you lose and gain weight, has also been linked to increased cancer risk. Crash diets or unmindful use of diet medications don’t work, either. Always check with your healthcare provider on what is best for you. If everything else fails, consider bariatric surgery to improve your health and reduce obesity and cancer risk.
Author’s BIO: Lori Wade is a journalist from Louisville. She is a content writer who has experience in small editions. Lori is currently engaged in news and conceptual articles on the health and beauty industry. You can find her on LinkedIn. Hope you appreciate Lori’s useful insights!

